60 Strathallen Avenue, Northbridge NSW
Monday to Friday - 9am to 5pm
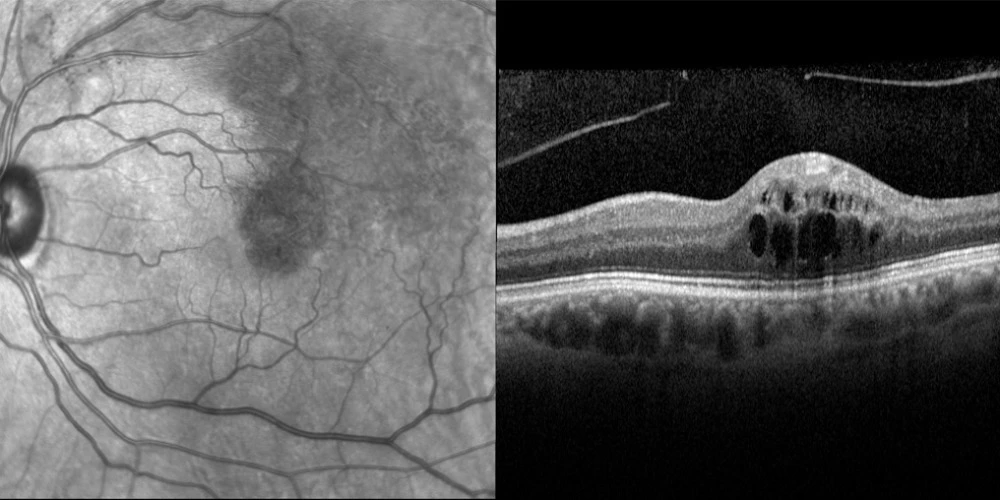
Branch Retinal Vein Occlusion (BRVO)
Branch Retinal Vein Occlusion is the second most common retinal vascular disease behind diabetic retinopathy. Most patients require a combination of injections and laser.
What is it?
A branch retinal vein occlusion is a blockage to one of the veins that drains blood out of the retina.
The blockage leads to a buildup in pressure on the vein, which causes haemorrhaging and fluid leaking out onto the retina. BRVO’s are the second most common retinal vascular disease behind diabetic retinopathy.
In most cases the blockage occurs at a point where an artery and vein cross. Thickening of the wall of the artery (from high blood pressure, high cholesterol, smoking or diabetes) applies pressure onto the vein and a blockage occurs at this point. Other risk factors for branch retinal vein occlusion may include glaucoma.
Symptoms
Symptoms for BRVO vary from person to person, depending where the blockage occurs.
If the blockage does not involve the macula a person may not even know it is there. For those that do involve the macula, symptoms may include:
- A sudden painless decrease or blurring of vision
- Part of their vision missing or black spots appearing in your vision.
- Distortion of vision
Diagnosis
Two special tests are used to diagnose BRVO.
A fluorescein angiogram is usually performed to identify the severity of impairment in retinal blood flow. The angiogram procedure involves a dye being injected into your arm and will be explained in detail. OCT (optical coherence tomography) is a scan to assess the presence or absence of macula oedema. This has no side effects.
Complications
There are two types of complications that can threaten vision in BRVO.
Macula oedema
This occurs when the occluded vein is near the macula. The leakage and bleeding causes the macula to swell leading to blurred vision and parts of vision missing.
Neovascularisation
In severe cases of BRVO, blood flow is sufficiently impaired such that the body responds by growing new, abnormal vessels. These abnormal vessels may grow into the vitreous where they can burst and bleed. This process is called neovascularisation and has the greatest potential to destroy vision.
Treatment
Several treatment methods are available to deal with macula oedema and to prevent neovascularisation.
Laser photocoagulation
Laser treatment can treat both macula oedema and prevent/treat the development of abnormal blood vessels.
In cases of macula oedema, the laser is focused on small areas around the macula where the leakage has occurred.
Where retinal ischaemia is prevalent, and there is a risk of neovascularisation, large areas of retina are treated by laser. The aim is to prevent the abnormal vessels from growing and the potential vision loss associated with the growth.
Intraocular injections
A type of medication called an anti-VEGF (Vascular Endothelial Growth Factor) treats both macula oedema and stops the growth of abnormal blood vessels. Repeat injections (approximately 4-6) are usually required. These usually occur approximately every 6 weeks. The thought of an injection into the eye may sound daunting but it is relatively painless and quick.
Most patients require a combination of injections and laser. This treatment of macula oedema may take 12-24 months. Although some patients stabilise earlier (6 months), four injections are standard to start the treatment. If the macula restores, then the duration between injections is stretched until injections are eased.
Has someone found a BRVO in your eye? At Northern Sydney Cataract, we are here to help!
If you have specific questions, please call our friendly staff on 02 9958 0552 or email us at info@nscataract.com.au
For appointments and enquiries, please phone 02 9958 0552
Monday to Friday 9am - 5pm
© 2015– Northern Sydney Cataract | Privacy Policy | Disclaimer | Website by: